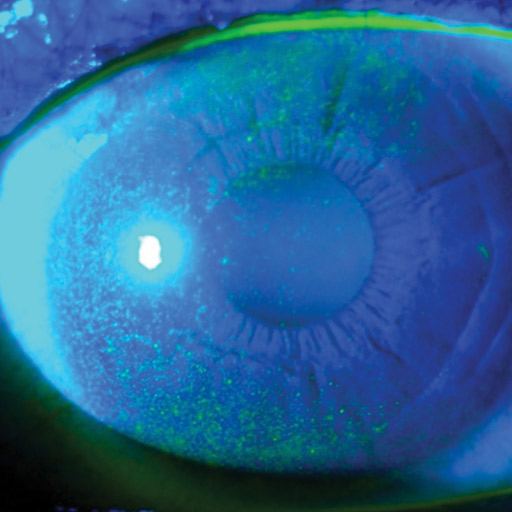
This condition is also known as Keratoconjunctivitis Sicca, but more commonly referred to as Dry Eye Disease (DED). The tear layer is made up of three layers; a lipid, aqueous and mucin layer; which becomes deficient in one or more of the layers. Systemic conditions, medications and environmental factors, like PCs and aircons often result in DED. The most common treatment of DED is the instillation of tear supplements combined with the implementation of a good lid cleaning regimen. The constant dry eye leads to micro erosions occurring on the corneal surface, and these micro breaks are an easy route into the cornea for various organisms leading to constant infections, and in some cases, severe conditions requiring urgent intervention.
Signs and Symptoms
Sometimes, dry eyes create too many tears. This confusing condition is called reflex tearing. It happens because the lack of moisture irritates your eye. It sends a distress signal through your nervous system for more lubrication. Your body sends a flood of tears to try to make up for the dryness. It’s a lot like what happens when you get sand in your eye and it runs. But these tears are mostly water, so they don’t act like normal tears. They can wash debris away, but they can’t coat your eye’s surface.
Dry eye symptoms may include any of the following:
- stinging or burning of the eye.
- a sandy or gritty feeling as if something is in the eye.
- episodes of excess tears following very dry eye periods.
- a stringy discharge from the eye.
- pain and redness of the eye.
- episodes of blurred vision.
- heavy eyelids.
- inability to cry when emotionally stressed.
- uncomfortable contact lenses.
- decreased tolerance of reading, working on the computer, or any activity that requires sustained visual attention.
- eye fatigue.
Causes and Risks
Typical common causes of chronic Dry Eye mostly include:
- Side effects of some medications, including antihistamines, nasal decongestants, tranquilizers, certain blood pressure medicines, Parkinson’s medications, birth control pills and anti-depressants.
- Skin disease on or around the eyelids.
- Meibomian gland dysfunction.
- In women during pregnancy.
- Women who are on hormone replacement therapy.
- Women taking only estrogen are 70 percent more likely to experience dry eye, whereas those taking estrogen and progesterone have a 30 percent increased risk of developing dry eye.
- After Lasik refractive surgery.
- Chemical and thermal burns.
- Chronic allergies.
- Infrequent blinking, associated with long hours working on computer or video screens.
- Both excessive and insufficient dosages of vitamins can contribute to dry eye.
- Homeopathic remedies may have an adverse impact on a dry eye condition.
- Loss of sensation in the cornea from long-term contact lens wear.
- Immune system disorders such as Sjögren’s syndrome, lupus, and rheumatoid arthritis.
- Chronic inflammation of the conjunctiva, or the lacrimal gland.
- If the surface area of the eye is increased, as in thyroid disease when the eye protrudes forward or after cosmetic surgery.
- Exposure keratitis (eyelids do not close completely during sleep).
Several risk factors for the development of Dry Eye Disease have been identified repeatedly in epidemiological studies, such as increasing age and female sex (particularly postmenopausal women). In clinical experience, menopausal and postmenopausal women both tend to have dry eye symptoms; this can be attributed to the significant decrease of tear production around the sixth decade of life in women. Hormonal studies suggest that sex hormones influence ocular surface conditions through their effects on tear secretions, meibomian gland function, and conjunctival goblet cell density. A study pointed out that women who were taking oral contraceptives had significantly higher goblet cell density than those who were not taking oral contraceptives. This was particularly true for women who used estrogen alone.
Stats and Incidence
Elderly people frequently experience dryness of the eyes, but dry eye can occur at any age. Nearly five million Americans 50 years of age and older are estimated to have dry eye. Of these, more than three million are women and more than one and a half million are men. Tens of millions more have less severe symptoms. Dry eye is more common after menopause. Women who experience menopause prematurely are more likely to have eye surface damage from dry eye.
Keratoconjunctivitis sicca is relatively common within the United States, especially so in older patients. Specifically, the persons most likely to be affected by dry eyes are those aged 40 or older. Keratoconjunctivitis sicca is estimated to affect 10% to 20% of adults, with 1 to 4 million aged 65 to 84 affected in the United States.
While persons with autoimmune diseases have a high likelihood of having dry eyes, most persons with dry eyes do not have an autoimmune disease. Instances of Sjögren syndrome and keratoconjunctivitis sicca associated with it are present much more commonly in women, with a ratio of 9:1. In addition, milder forms of keratoconjunctivitis sicca also are more common in women. This is partly because hormonal changes, such as those that occur in pregnancy, menstruation, and menopause, can decrease tear production.
In areas of the world where malnutrition is common, vitamin A deficiency is a common cause. This is rare in the United States.
Racial predilections do not exist for this disease
Treatment
Artificial tear drops and ointments are the most common treatment. Many types of drops are available. No one product works for everyone, so you might have to try a few to figure out the one that’s right for you. If you have chronic dry eye, you need to use the drops even when your eyes feel fine, or they won’t stay wet enough. If your eyes dry out while you sleep, you can use a thick product, like an ointment, at night.
If artificial tears do not adequately address these inflammatory changes, your doctor may recommend steroid eye drops to better manage the underlying inflammation associated with dry eyes. Steroid eye drops are generally used short-term to quickly manage symptoms. They are typically used in conjunction with artificial tears.
Punctal plugs are also an option. Small, sterile devices are inserted into one or both of the small openings (puncta) that are located in the inner corner of the upper and lower eyelids. After these openings have been plugged, tears can no longer drain away from the eye through these ducts. In this way the tear film stays intact longer on the surface of the eye.
A very significant percentage of dry eye cases are caused by inadequate oil (meibum) being secreted from meibomian glands located along the margin of the eyelids. Gently massaging the eyelids can aid the release of the oily component of the tear layer. An alternative (and potentially more comfortable) way to help open clogged meibomian glands to treat dry eyes is to simply apply warm compresses to the closed eyelids to soften the hardened meibum.
Studies have found that supplements containing omega-3 fatty acids can decrease dry eye symptoms. Good sources of omega-3s include cold-water fish such as salmon, sardines, herring and cod. For a vegetarian source of omega-3s, flaxseed oil can help to relieve dry eye.
In extreme cases, surgical cautery is a procedure to permanently seal the ducts of the lacrimal drainage system
If you have mild dry eye symptoms be sure to:
- Blink more frequently.
- Take frequent breaks during computer use.
- Remove eye makeup thoroughly.
- Clean your eyelids.
- Wear quality sunglasses.