Overview
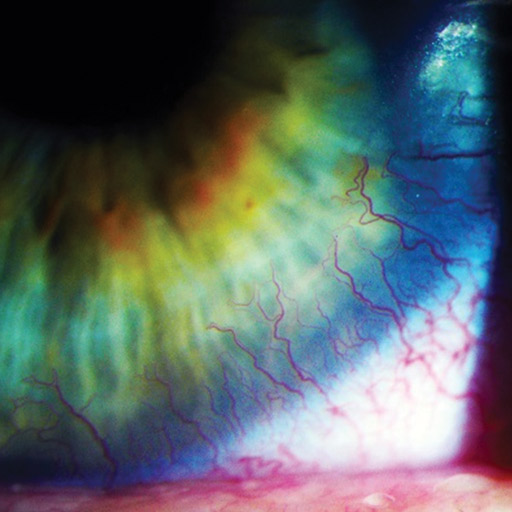
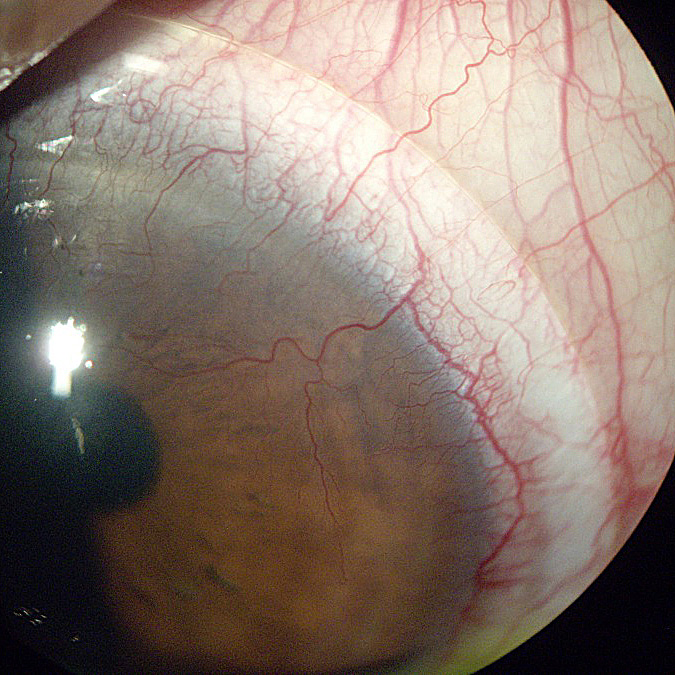
Corneal Neovascularization can be defined as the excessive growth of blood vessels that occurs at the level of the cornea. The main cause of the problem is represented by the oxygen deprivation. In healthy individuals, the cornea is transparent and it lacks vascularization. Both ocular insults and ocular hypoxia are responsible for the appearance of corneal vascularization.
The condition is often encountered in those who wear contact lenses. Risk factors for the appearance of corneal neovascularization include high myopia, the dry eye syndrome and different conditions with ocular involvement (compromised immune system, Sjögren’s syndrome or acne rosacea). Hydrogel contact lenses present the highest risk for corneal neovascularization.
If the progression of vessels persists, reduced wearing time is the first course of action, and careful monitoring of the progression by your eyecare professional is essential. In some cases, rigid gas permeable (hard lenses) are an option to slow down the progression. If, in extreme cases, the progression is not contained, one may have to refrain from wearing contact lenses altogether.
This condition is not life-threatening but it can lead to loss of vision in more severe cases. The vision can be threatened by the direct invasion of the blood vessels at the level of the cornea or because of secondary changes, such as the haemorrhage or scarring.
It can be stopped or slowed down by decreasing contact lens wear. But if it is very significant, the only treatment is corneal transplant surgery.
Signs and Symptoms
During a routine eye exam, the following changes can be identified
- Limbal hyperemia (Redness around the cornea) – earliest sign of corneal neovascularization.
- Superficial vessels identified at the level of the cornea (single or multiple).
- In the situation that the deep stromal vessels are responsible for the corneal neovascularization, these are identified at the level of the cornea (sometimes accompanied by nerve fibres).
- Active engorged vessels and lipid exudate.
- Light sensitivity.
- Decreased vision or blurring when wearing contact lenses.
- Intolerance to contact lens after wearing them for a short time.
- Corneal edema and leakage.
- Lipid deposition – yellow-white opacities (surround the stromal vessels).
Causes and Risks
These are the most common causes that lead to corneal neovascularization
- Wearing contact lenses.
- Viral infection (Common – herpes simplex).
- Corneal ulcers.
- Infectious keratitis.
- Immunological conditions.
- Corneal trauma.
- Alkali injury.
Risk factors that can increase the risk for corneal neovascularization are
- poor compliance.
- inadequate hygiene of the contact lenses.
- poor follow-up care.
The invasion of the cornea by the deep stromal vessels presents the biggest risks, with the optical transparency being lost due to a series of changes. Among the most important changes, there are the hemorrhage and scarring that can occur at the level of the cornea. The deposits of lipids can also affect the optical transparency, complicating the already existent corneal neovascularization.
Complications
Left untreated, the corneal neovascularization can progress and have a negative impact on the eyesight. Those who wear contact lenses should visit their eye care practitioner on an annual basis, for a routine eye exam.
Stats and Incidence
There is no age, race or gender predilection for the corneal neovascularization to have been identified so far
Treatment
A study performed on lab rats has demonstrated that both triamcinolone and doxycycline can be used to reduce the neovascularization process at the level of the cornea (topical instillation). Other studies recommend using angiotensin II receptor blocker drug telmisartan as a prophylactic measure (prevention of corneal neovascularization). The topical application of bevacizumab (anti-VEGF) has also been recommended as a treatment for corneal neovascularization.
Other treatment measures include
- Discontinuing the current contact lenses and replacing them with better ones (higher oxygen permeability).
- Refitting the current contact lenses.
- Permanent discontinuation of the contact lenses in patients diagnosed with severe forms of corneal neovascularization (reducing the risk of losing one’s eyesight).
- Treatment of the underlying cause or of the associated conditions (acne rosacea, dry eye syndrome, blepharitis, viral or bacterial infections – particularly those with staphylococcus).
- Topical corticosteroids for active neovascularization.
- Superficial keratectomy is recommended in combination with topical and subconjunctival bevacizumab.
- Corneal transplantation for patients who present with central corneal scarring, however they present a high risk for rejection in severe cases of corneal neovascularization.
- Photodynamic therapy.
- Argon laser obliteration performed at the level of the vessel lumen.
- Hyperbaric oxygen treatment, but with limited success.
- Amniotic membrane transplantation for the regeneration of the ocular surface.